TRENDS IN EMERGENCY DEPARTMENT UTILIZATION AND OPTIMIZATION: PART 1 OF 3
- Jonathan Rogg, MD, MBA
- 01/28/2020
I aspire toward making all trips to the emergency room a little less painful, starting with my own patients, but ideally everywhere. I have dedicated my career to researching and adopting practices that lead to operational improvement, while teaching others how to bring those techniques to their own organizations. I have a keen interest in using technology for process improvement and pursuit of clinical excellence.
In this series of short articles, I will explore the explosion of ED use in our healthcare system, some of the barriers associated with operational excellence in the ED, and perhaps most importantly, ending with some suggestions for best practices. This initial article will set the stage and explain the current trends in ED utilization and to remind all of us how central the ED is to many of our healthcare-related needs.
With each passing year EDs become busier. Although exact health utilization statistics tend to lag current trends, historical data show that utilization of the ED continues to grow both in total number of patient visits and overall rate of utilization. Let me start by sharing some numbers with you that should make it clear that you, or a loved one, is likely going to visit an ED at some point in the near future if you haven’t already in the recent past.
Between 2001 and 2016, the number of ED visits increased from 107.5 million to 146.6 million per year. While a portion of this increased utilization can be attributed to an overall increase in population, what is more striking is that the rate of utilization per 1,000 people has increased substantially as well. Between 1995 and 2016 the utilization rate per 1,000 people increased from 369 to 458.1 In other words, one out of every two people in the U.S. will visit an ED this year. Of course, there are certain populations that continue to be high utilizers: infants (children under the age of 1), the elderly, the chronically ill, and the homeless. However, the overall numbers suggest that ED use is increasing for all Americans. The chart below looks at the utilization trends for a 10-year period, starting in 2006 and ending in 2016, for several different age cohorts. As one can see, the trends are clearly pointing up across nearly every age demographic.2
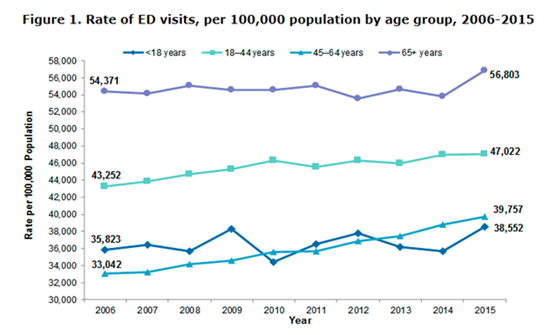
Source: Agency for Healthcare Research and Quality (AHRQ), Center for Delivery, Organization, and Markets. Healthcare Cost and Utilization Project (HCUP), Nationwide Emergency Department Sample (NEDS), 2006–2015
The reality is that, in 2016, about 69% of all patients admitted to the hospital initially came in through the ED. Consider this number again: 458 visits per 1,000 people per year in 2016 with trends suggesting an even higher rate likely in 2020.
The rise of ED utilization matters whether we are currently healthy or not. At some point, a visit to the ED for ourselves or with a family member is inevitable. Whether the ever-increasing use of the ED is clinically appropriate, good or bad from a policy perspective, financially sound or not, is a topic of endless debate that is beyond the scope of this article. Being a patient in the ED is scary and stressful. ED patients are often in pain. Consider your own feelings about an ED experience or the notion of having to spend time in one. As you think about it, consider how you would answer some of these questions: did you see a physician in a reasonably timely fashion? If you received any diagnostic testing, how long did it take? Did you have a battery of tests? Were they necessary? What was the turnaround on getting the results? What was your experience with the physician(s), nurse(s), and the rest of the clinical staff? If you needed to be hospitalized, how long did it take for that decision to be made and for you to be transferred to a hospital bed?
If your responses were mostly positive and your expectations were met, then you were lucky enough to encounter a well-run ED—something that requires a tremendous amount of effort, coordination, and implementation of data-driven best practices.
My guess is that a sizable majority of you likely had an ED experience that was less than ideal. This could be because of a number of factors. Some are external to the emergency department, such as the time of day and the day of the week (Monday afternoons are usually busiest). Some are hospital-level factors such as inpatient room availability. However, many ED-specific factors were very likely to have had a significant impact on your experience and the care that you received. Did that emergency department invest the time, money, and energy into the necessary systems and technology to ensure that everybody is well-aligned, communicating, and working towards the same goals and performance metrics? It requires an open mind and a willingness to embrace process change.
What is the benefit of a well-run emergency department? The data that we will be exploring in the next article in this series, suggests that the difference between a well-run ED versus one that is overcrowded, inefficient, disorganized, reliant on redundant testing, mired in unnecessary delay, etc. can literally be the difference between life and death. It is my personal mission as a physician, an educator, and an administrator to ensure that my EDs are equipped to deliver the high level of care that we would all expect to receive. This is particularly crucial as the ED becomes an increasingly ubiquitous way that we access care. Emergency departments must use innovative techniques and the best medical evidence to ensure high quality, efficient emergency care is available when you need it.
Please join me next time when I go a layer deeper to explore the structural and operational differences that make an emergency department well positioned to deliver exceptional care. Until then, stay healthy and out of the ED!
Best,
Jon
1.Augustine, J. The Latest Emergency Department Utilization Numbers Are In. October 20, 2019. American College of Emergency Medicine. https://www.acepnow.com/article/the-latest-emergency-department-utilization-numbers-are-in/?singlepage=1
2. Sun R (AHRQ), Karaca Z (AHRQ), Wong HS (AHRQ). Trends in Hospital Emergency Department Visits by Age and Payer, 2006–2015. HCUP Statistical Brief #238. March 2018. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/reports/statbriefs/sb238-Emergency-Department-Age-Payer-2006-2015.pdf.
About Author

Jonathan Rogg, MD, MBA
Jonathan is an academic emergency physician and expert in hospital operations with several related publications. He is Vice Chair of Strategy and Operations at McGovern Medical School, part of UTHealth in Houston. Jonathan completed his emergency medicine residency at Massachusetts General Hospital, and Brigham & Women’s Hospital, and earned an MBA from Harvard.
