INCREASING RATE OF DISCHARGE SUMMARIES BEFORE SNF TRANSFER
- John "JP" Pollard
- 11/13/2023
We have enjoyed a long partnership with a large not-for-profit health system serving portions of the eastern US coast. Earlier this year we put out a case study that highlights many of the successes we have shared with this organization. You can find that case study here.
Recently we were looking through some of the data in preparation for a quarterly business review, and the results for one particular insight stopped us in our tracks.
Briefly, what does Agathos do?
Before we continue, allow me to explain what we do so this will all make sense. Agathos shows physicians how their practice patterns compare to those of their peers. This piques their curiosity and sparks self-determined change that lowers the cost of care and improves patient outcomes. With Agathos, physicians receive one text once per week with a seamless link to a web-based application featuring their individualized data about a specific practice pattern (e.g., telemetry utilization, common lab orders, timing of PT/OT consults). They can see how they practice relative to their peers within their hospital, review historical trends, and view recent case examples featuring the relevant practice in the metric. In our previous work with this organization, the Agathos program produced physician engagement, group collaboration, and practice change within the hospital medicine team.
The “insight” that impressed us
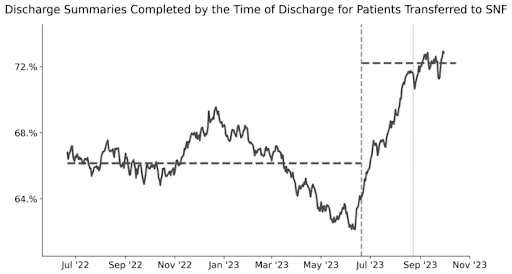
Now, onto the specific metric that impressed us. The “insight” is called “Discharge Summaries Completed by the Time of Discharge for Patients Transferred to SNF.” (Whew! That is one long name!)
Setting the context
For context, throughout 2023, a major focus across all of the organization’s campuses was increasing rates of timely (i.e., within 24 hours of discharge) discharge summary completion. Prior to Agathos, there was some focus regarding skilled nursing facility (SNF) transfers and discharge summaries being complete yet earlier — at the time of discharge — but without the success they had hoped for. This goal incrementally aids seamless transitions of care, with associated benefits on LOS, readmissions [each for the hospital], and other patient outcomes [including at the SNF].
Results
We started sending this particular insight in June and have already seen an increase in the rate of discharge summaries completed at the time of discharge for patients discharged to SNF. The chart below shows the change in physician practice after only two sends of this insight.
Apart from the change (impressive in and of itself), this example is noteworthy for a number of reasons more broadly applicable to physician practice improvement.
First, this was at least the twentieth insight released with these hospitalists. Scaling and sustaining metrics is difficult, and often it can be tempting to just “pick a few and focus on them,” yet medicine — at least at the practice level— is not like that. Each day physicians may make dozens of different actions and decisions, and some of the greatest opportunities may be hidden by summary-level approaches to practice data, and at any rate the sum of opportunity will vary by physician, facility, patient population, or season.
Second, SNF optimization (i.e., all disposition, efficiency metrics, process adherence) had been an organizational focus for some time, yet physicians were justifiably not bought into the global metrics already in place, such as SNF utilization rate or LOS [for SNF-discharged patients]. They rightly pointed out the many factors that rolled up into these higher-level indicators, many outside their control, and they asked for metrics that a hospitalist could act upon. The above insight was one of the fruits of that feedback. Evidently the newfound buy-in was immediate.
Third, and not uniquely to this insight (yet a great example), this is quality insight — process adherence — that has inherent outcomes impact. Many data approaches start and stop at outcomes, or they might feature utilization trends of scarce resources (whether labs, telemetry, or SNFs in this case) of value to hospital and patient. One might argue there are too many quality items (see point #1), and why zoom into them if they are not intrinsically valuable [apart from their outcomes]?
However, in contrast to outcomes and even utilization metrics (see point #2), physicians are bought into quality metrics. If they see a “do” or “don’t” that their peers are doing more or less frequently than them, there is not a lot of convincing to do. They want to change, and repeat enough positive experiences with that, and outcomes improve. There may even be a bit more buy-in and curiosity to the factors driving cost and outcomes data previously ignored.
In summary
We are proud of the impact that Agathos Enterprise has had for this specific insight and others. This is, again, just one insight of dozens that are available in each of our insight Libraries (i.e., Hospital Medicine, Emergency Medicine, Primary Care). You can learn more about the other areas where we realized success in our case study.
Should any of this pique your interest, give us a call and we can discuss what these interventions might look like at your healthcare organization. 
About Author

John "JP" Pollard
JP has over 25 years of marketing experience ranging from executive and product management roles to leadership at award-winning agencies. He has marketed for American Airlines’ SABRE division, SAP’s Germany-based services organization, and also for startups in supply chain technology and healthcare. Prior to joining Agathos in October 2021, JP was VP of marketing for healthcare consulting firm Nordic Consulting Partners (now Nordic Global).

